 This week, JAMA Surgery published the final results of the Mastectomy Reconstruction Outcomes Consortium (MROC) — the first comprehensive look at how cancer patients fare (physically and emotionally) after breast reconstruction. The New York Times had excellent coverage (aside from the cringe-inducing ending).
This week, JAMA Surgery published the final results of the Mastectomy Reconstruction Outcomes Consortium (MROC) — the first comprehensive look at how cancer patients fare (physically and emotionally) after breast reconstruction. The New York Times had excellent coverage (aside from the cringe-inducing ending).
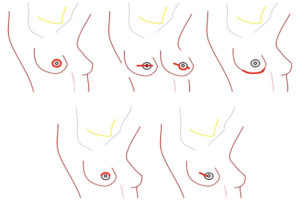
Quick summary: MROC researchers looked at 8 different breast reconstructive procedures performed by 57 different surgeons at 11 sites across the US and Canada. They enrolled 2,224 patients and followed them for four years.
Last month, I spoke with Ed Wilkins, MD, MROC’s lead author and a plastic surgeon at the University of Michigan in Ann Arbor. “We designed and conducted MROC because the decision to reconstruct isn’t just one decision, it’s a constellation of decisions,” he said. “And our patients were getting lost.”

